Tag: RFK Jr.
-

Is Web3 Ready To Revolutionize Healthcare?
Late last year, the U.S. Department of Health and Human Services (HHS) took a bold step toward modernizing healthcare data exchange by finalizing The Trusted Exchange Framework and Common Agreement (TEFCA). This initiative aimed to enhance equity, innovation, and interoperability by facilitating the secure exchange of electronic health records (EHRs). At its core, TEFCA sought…
-
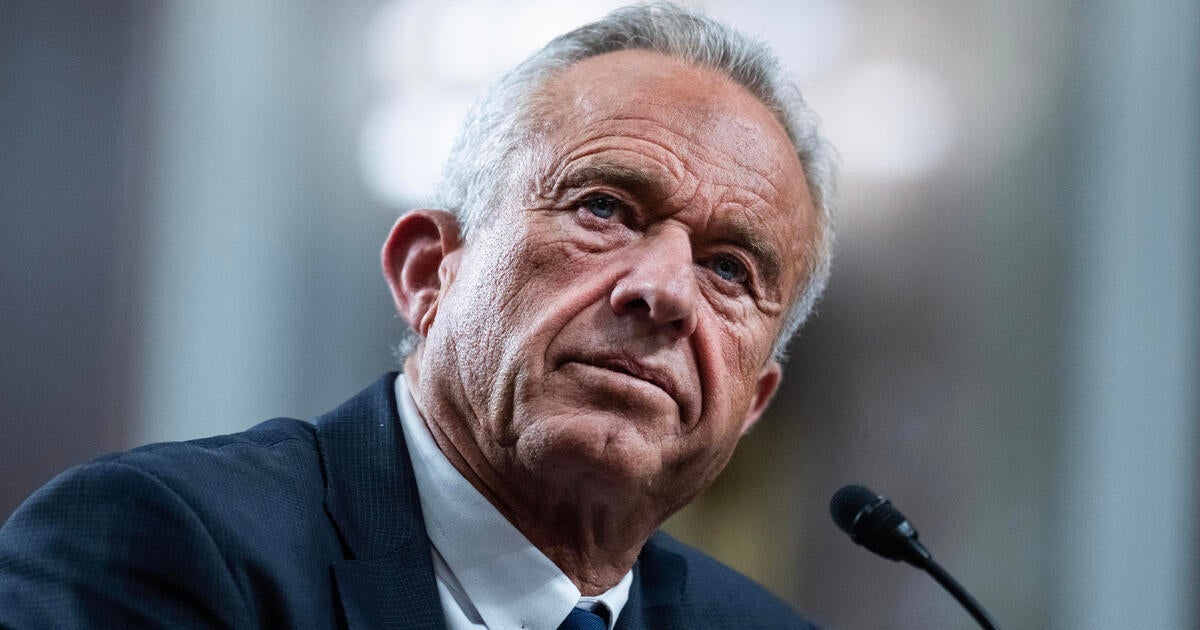
RFK Jr. rolls back transparency policy on Medicaid and NIH changes
Health and Human Services Secretary Robert F. Kennedy Jr. ended a longstanding transparency rule on Friday, supercharging his authority to change policies in areas ranging from Medicaid to the National Institutes of Health without advance notice to the public. Dubbed the “Richardson Waiver” after the former health secretary who issued the rule in 1971, the…